Dr. Alexander Abkin Recognized as a New Jersey Top Doctor in Bariatric Surgery for 2025
Dr. Alexander Abkin, renowned New Jersey bariatric surgeon, has once again been recognized as a New Jersey Top Doctor in Bariatric Surgery for 2025 by New Jersey Monthly Magazine. This prestigious honor marks the 18th consecutive year that Dr. Abkin has earned this distinction, underscoring his exceptional expertise and unwavering commitment to improving the health and well-being of his patients through life-changing weight loss surgery.
Dr. Abkin’s recognition in the New Jersey Monthly survey is a result of peer nominations, where physicians across the state vote for their colleagues who demonstrate excellence in their specialty. Being named to this list year after year highlights Dr. Abkin’s standing as a leader in bariatric surgery and his dedication to delivering the highest standard of care to individuals seeking sustainable weight loss solutions.
“Being recognized as a Top Doctor is a great honor, and I am deeply grateful for the trust my patients and fellow physicians have placed in me over the years,” said Dr. Abkin. “My goal has always been to provide compassionate, individualized care that not only helps my patients achieve their weight loss goals but also empowers them to lead healthier, more fulfilling lives.”
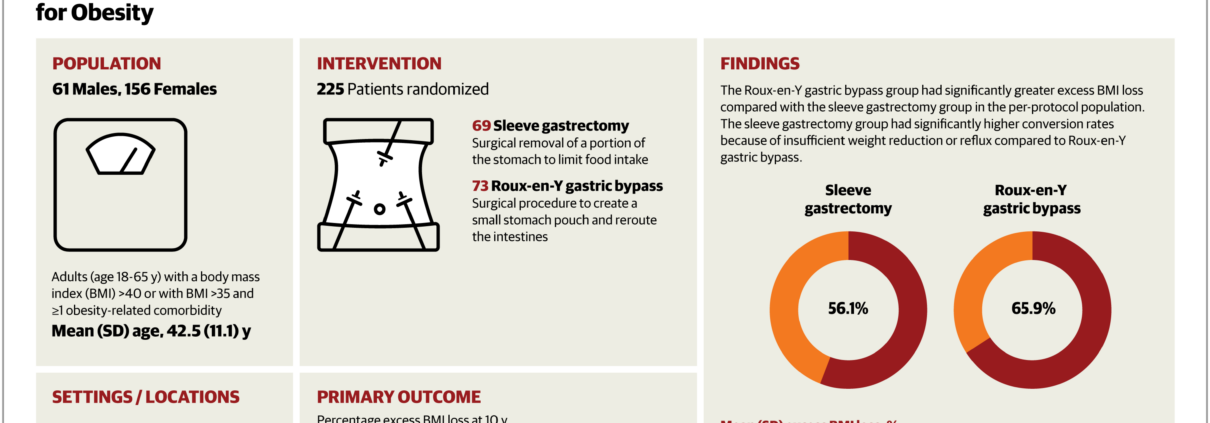
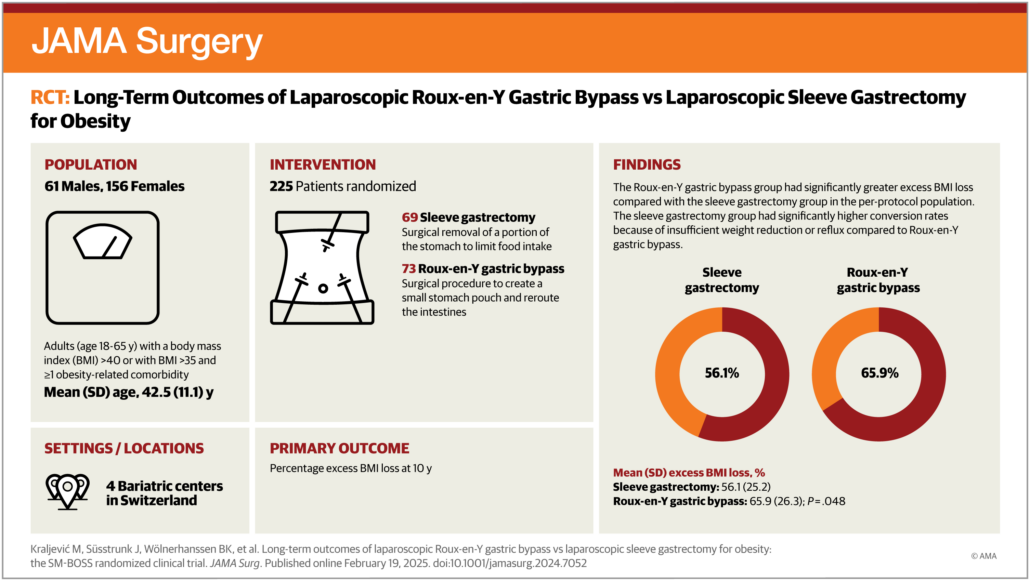
Dr. Abkin is highly respected in the field of bariatric surgery, specializing in laparoscopic procedures, weight loss surgery, and minimally invasive techniques. He is known for his expertise in both gastric bypass and sleeve gastrectomy procedures, as well as his comprehensive approach to patient care that includes pre- and post-surgery support.
Throughout his career, Dr. Abkin has earned a reputation for his innovative approach, which combines cutting-edge technology with a deep understanding of his patients’ unique needs. His practice is dedicated to providing personalized care that addresses not only the physical aspects of weight loss but also the psychological and emotional challenges that accompany the journey.
Dr. Abkin is also an active member of several professional organizations, including the American Society for Metabolic and Bariatric Surgery (ASMBS), and regularly participates in research, education, and speaking engagements to advance the field of bariatric surgery.
About Dr. Alexander Abkin
Dr. Alexander Abkin is a board-certified bariatric surgeon with over two and a half decades of experience in weight loss surgery. He is a pioneer in minimally invasive techniques and has performed thousands of successful surgeries. Dr. Abkin is dedicated to providing patients with compassionate care and a path to lasting health transformation. He practices in Florham Park, Edison and Paramus, where he and his team offer a comprehensive suite of services, including bariatric surgery, nutritional counseling, and long-term patient support.
For more information about Dr. Abkin’s practice or to schedule a consultation, please call 973-410-9700.